Trigeminal neuralgia is a chronic pain condition that affects the trigeminal nerve, which carries sensation from your face to your brain. Even mild stimulation of your face—such as brushing your teeth or putting on makeup—can trigger a jolt of excruciating pain. The pain can be so severe that it affects your quality of life. Fortunately, there are various treatment options available to help manage and alleviate the pain associated with this condition. In this comprehensive guide, we will explore the most effective treatments for trigeminal neuralgia, ranging from medication to surgical options, and offer insights into finding the right approach for your needs.
Understanding Trigeminal Neuralgia
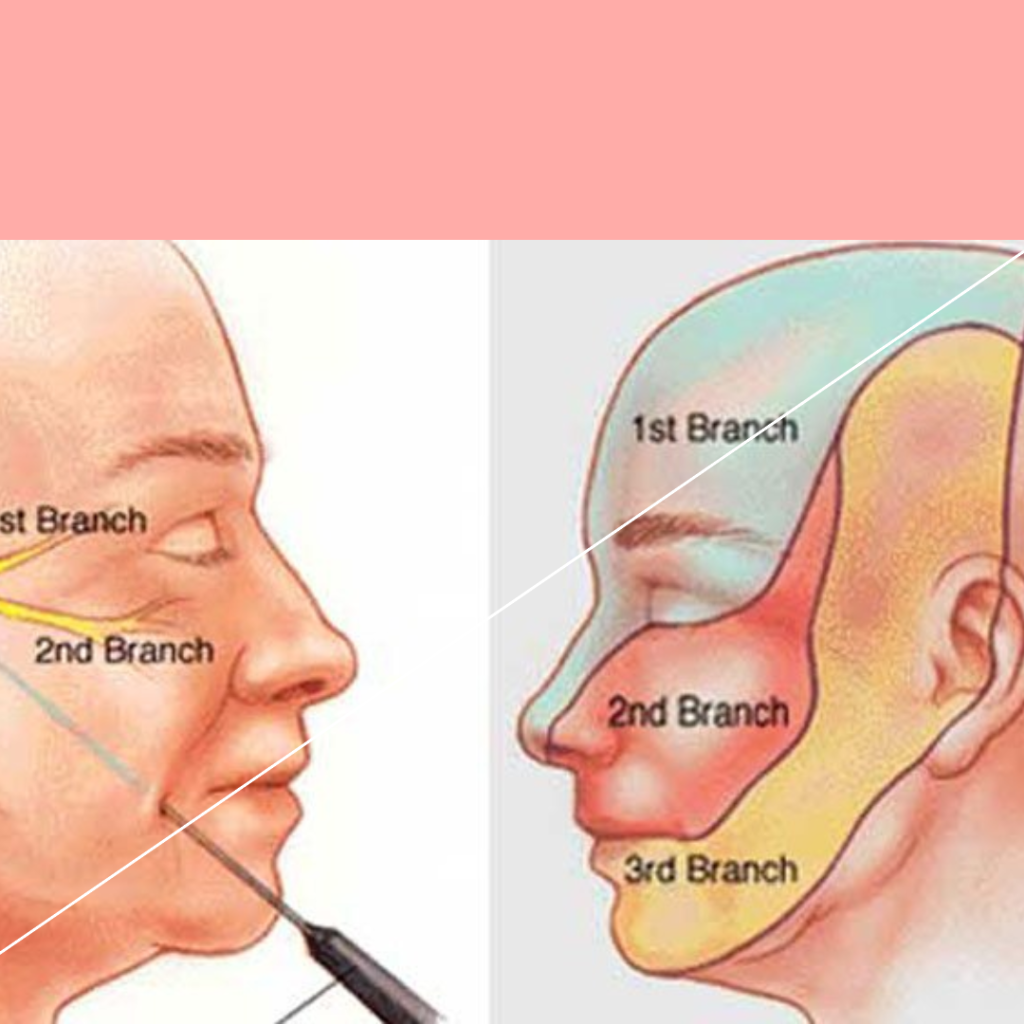
Trigeminal neuralgia, also known as tic douloureux, is a chronic pain condition that affects the trigeminal nerve, one of the most widely distributed nerves in the head. It is characterized by sudden, severe, and stabbing pain in the areas supplied by the trigeminal nerve, including the cheeks, jaw, teeth, gums, lips, and sometimes the eyes and forehead. Understanding the underlying causes and symptoms of this condition is crucial for effective diagnosis and treatment.
Causes of Trigeminal Neuralgia
The exact cause of trigeminal neuralgia is not always clear, but it is often related to the following factors:
Nerve Compression: The most common cause is blood vessels pressing on the trigeminal nerve as it exits the brainstem. This compression wears away the protective coating around the nerve (myelin sheath), leading to erratic and hyperactive nerve signals.
Multiple Sclerosis (MS): In some cases, trigeminal neuralgia is associated with MS, a disease that damages the myelin sheath in the central nervous system.
Tumors: Rarely, tumors pressing on the trigeminal nerve can cause trigeminal neuralgia.
Injury or Trauma: Facial or dental trauma or surgical procedures can sometimes damage the trigeminal nerve, leading to this condition.
Common Symptoms and Diagnosis
Recognizing the symptoms of trigeminal neuralgia is vital for early diagnosis and management. The most common symptoms include:
Pain Episodes: Sudden, severe, and shock-like pain that may feel like an electric shock. These episodes can last from a few seconds to several minutes and can occur spontaneously or be triggered by activities such as eating, talking, or touching the face.
Triggers: Common triggers include light touch, facial movements, chewing, brushing teeth, or even a gentle breeze.
Pain Distribution: The pain usually affects one side of the face, though in rare cases, it can affect both sides.
Diagnosis: Diagnosis typically involves a detailed medical history, neurological examination, and imaging tests like MRI to rule out other conditions. Electrophysiological tests may also be conducted to assess nerve function.
Medication-Based Treatments
Medications are often the first line of treatment for managing trigeminal neuralgia. These drugs can help control the pain by stabilizing the nerve activity. While medications may not provide a permanent cure, they can significantly improve the quality of life for many patients.
Anticonvulsants and Their Role
Anticonvulsants are commonly used to treat trigeminal neuralgia because they help reduce nerve pain by slowing down nerve impulses. Some of the most frequently prescribed anticonvulsants include:
Carbamazepine (Tegretol): This is often the first choice for treating trigeminal neuralgia. It is effective in reducing or eliminating pain in many patients. However, it can have side effects such as dizziness, drowsiness, and nausea.
Oxcarbazepine (Trileptal): Similar to carbamazepine, oxcarbazepine is another effective anticonvulsant with fewer side effects. It is often prescribed when patients cannot tolerate carbamazepine.
Other Anticonvulsants: Other drugs such as gabapentin (Neurontin) and lamotrigine (Lamictal) may be used, particularly if patients do not respond well to the first-line treatments.
Pain Relievers and Other Pharmaceuticals
In addition to anticonvulsants, other medications can be used to manage the pain associated with trigeminal neuralgia:
Tricyclic Antidepressants: Medications such as amitriptyline and nortriptyline can be effective for managing chronic pain. They are often used in combination with anticonvulsants.
Muscle Relaxants: Drugs like baclofen can help relieve muscle tension that might contribute to pain. They are sometimes used in combination with other medications.
Topical Treatments: Topical anesthetics such as lidocaine patches or creams can provide localized pain relief without systemic side effects.
Surgical Treatment Options
When medications fail to provide adequate relief or cause intolerable side effects, surgical treatments may be considered. Surgical options aim to alleviate pain by addressing the underlying cause, such as nerve compression or damage.
Microvascular Decompression (MVD)
Microvascular decompression (MVD) is a surgical procedure that involves relieving pressure on the trigeminal nerve by repositioning or removing blood vessels that are compressing the nerve.
Procedure Details: During MVD, a surgeon makes a small incision behind the ear and removes a small piece of the skull to access the nerve. The surgeon then moves or removes the blood vessels pressing on the nerve, placing a small pad between the nerve and the vessels to prevent future compression.
Benefits and Risks: MVD is highly effective in providing long-term pain relief for many patients. However, as with any surgical procedure, it carries risks such as infection, hearing loss, and stroke.
Stereotactic Radiosurgery (Gamma Knife)
Stereotactic radiosurgery, commonly known as Gamma Knife surgery, is a non-invasive procedure that uses focused radiation to damage the trigeminal nerve and reduce pain signals.
Procedure Details: Gamma Knife surgery involves delivering precise, high-dose radiation beams to the trigeminal nerve without making any incisions. The procedure is performed on an outpatient basis and usually takes one to two hours.
Benefits and Risks: This treatment is effective for many patients, offering pain relief with minimal risk of complications. However, pain relief may not be immediate, and some patients may experience a recurrence of symptoms over time.
Non-Surgical and Alternative Therapies
For patients who prefer to avoid surgery or those who do not find sufficient relief from medications, non-surgical and alternative therapies can offer additional options for managing trigeminal neuralgia.
Physical Therapy and Exercises
Physical therapy can help alleviate the pain and improve the overall well-being of patients with trigeminal neuralgia. Various exercises and techniques are used to reduce muscle tension and improve blood flow.
Exercise Programs: Customized exercise programs, including facial exercises, neck stretches, and gentle aerobic activities, can help strengthen muscles and reduce pain.
Manual Therapy: Techniques such as massage, myofascial release, and trigger point therapy can help relieve muscle tension and improve circulation, which may reduce pain intensity.
Acupuncture and Herbal Remedies
Acupuncture and herbal remedies are often used as complementary therapies for managing trigeminal neuralgia. These approaches focus on balancing the body’s energy and promoting natural healing.
Acupuncture: This ancient Chinese practice involves inserting thin needles into specific points on the body to stimulate nerves, muscles, and connective tissue. Acupuncture is believed to help alleviate pain by releasing endorphins and improving blood flow.
Herbal Remedies: Various herbs such as St. John’s Wort, passionflower, and skullcap have been traditionally used to manage nerve pain. Herbal supplements can be used in conjunction with other treatments to enhance their effectiveness. However, it’s important to consult with a healthcare provider before starting any herbal regimen.
Lifestyle Changes and Pain Management Techniques
In addition to medical treatments and therapies, certain lifestyle changes and pain management techniques can help patients with trigeminal neuralgia manage their condition more effectively. These approaches focus on reducing triggers and improving overall well-being.
Diet and Nutrition
Diet and nutrition play a crucial role in managing trigeminal neuralgia. Certain foods can trigger nerve pain, while others can help reduce inflammation and promote nerve health.
Trigger Foods: Identifying and avoiding foods that trigger pain, such as caffeine, alcohol, and processed foods, can help manage symptoms. Keeping a food diary can help patients identify specific triggers.
Anti-Inflammatory Diet: Consuming a diet rich in anti-inflammatory foods, such as fruits, vegetables, omega-3 fatty acids, and whole grains, can help reduce inflammation and support nerve health.
Stress Management and Coping Strategies
Stress is a common trigger for trigeminal neuralgia pain. Effective stress management and coping strategies can help patients manage their condition and improve their quality of life.
Relaxation Techniques: Practices such as deep breathing exercises, meditation, and yoga can help reduce stress and promote relaxation, which may reduce the frequency and intensity of pain episodes.
Support Networks: Joining support groups and connecting with others who have trigeminal neuralgia can provide emotional support and practical advice for managing the condition. Counseling and therapy can also help patients develop coping strategies and manage anxiety and depression related to their condition.
Conclusion
Trigeminal neuralgia is a challenging condition that can significantly impact a person’s quality of life. However, with a comprehensive understanding of the available treatments, patients can find effective ways to manage their pain. From medications and surgical options to non-surgical therapies and lifestyle changes, there are various approaches to help alleviate the symptoms of trigeminal neuralgia. By working closely with healthcare professionals and exploring different treatment options, patients can develop a personalized plan that offers relief and improves their overall well-being.
Frequently Asked Questions (FAQs)
1. What are the most common triggers for trigeminal neuralgia pain?
Answer: Common triggers for trigeminal neuralgia pain include activities such as eating, talking, brushing teeth, and touching the face. Environmental factors like cold wind or a gentle breeze can also trigger pain episodes. Identifying and avoiding these triggers can help manage symptoms.
2. How effective are medications in treating trigeminal neuralgia?
Answer: Medications, particularly anticonvulsants like carbamazepine and oxcarbazepine, are often effective in managing trigeminal neuralgia pain. However, their effectiveness can vary from person to person, and some patients may experience side effects. Medications are typically the first line of treatment, but other options may be explored if they are not sufficient.
3. What are the risks associated with surgical treatments for trigeminal neuralgia?
Answer: Surgical treatments, such as Microvascular Decompression (MVD) and Stereotactic Radiosurgery (Gamma Knife), carry risks like any other surgical procedure. Potential risks include infection, hearing loss, stroke, and facial numbness. Despite these risks, many patients experience significant pain relief from these procedures.
4. Can lifestyle changes really make a difference in managing trigeminal neuralgia?
Answer: Yes, lifestyle changes can play a significant role in managing trigeminal neuralgia. Identifying and avoiding dietary triggers, practicing stress management techniques, and maintaining a healthy diet can help reduce the frequency and intensity of pain episodes. Combining these changes with medical treatments can enhance overall pain management.
5. Are there any non-surgical treatments that can provide long-term relief for trigeminal neuralgia?
Answer: Non-surgical treatments such as physical therapy, acupuncture, and herbal remedies can provide relief for some patients. While these treatments may not offer a permanent cure, they can help manage symptoms and improve quality of life. It is important to work with healthcare providers to find the most effective combination of treatments for long-term relief.Know more details visit here: NEURO SCIENCES CENTERS